Lähmungen des Plexus brachialis (Armplexus):
Der Armplexus besteht aus Nerven, die vom Rückenmark im Halswirbelbereich ausgehen und den gesamten Arm (incl. Schultergürtel, Oberarm, Unterarm und die Hand) motorisch und sensibel (Kraft und Gefühl) versorgen. Verletzungen von Nerven des Armplexus kommen häufig in einer jüngeren, sportlichen Patientengruppe vor (typisch nach Motorrad- oder Fahrradunfall, häufiger Männer als Frauen).
Man erkennt solche Schäden an Bewegungseinschränkungen in dem betroffenen Arm und Schultergürtel sowie auch durch Gefühlsstörungen in diesen Bereichen. In der Regel entstehen Lähmungen gleich nach dem Unfall. Abhängig von einzelnen Fällen kann es sich von einfacheren Dehnverletzungen oder Zerrungen bis zur Nervendurchtrennung oder Wurzelausriß in verschiedenen Höhen handeln. In der akuten Phase (bei geschlossenen Verletzungen) sollen solche Armplexuslähmungen aktiv mit physiotherapeutischen Maßnahmen unter engmaschigen neurologischen Kontrollen behandelt werden. Bei über drei bis vier Monate hinausgehenden persistierenden Lähmungen und Gefühlsstörungen sollten die chirurgischen Behandlungsmöglichkeiten berücksichtigt werden.
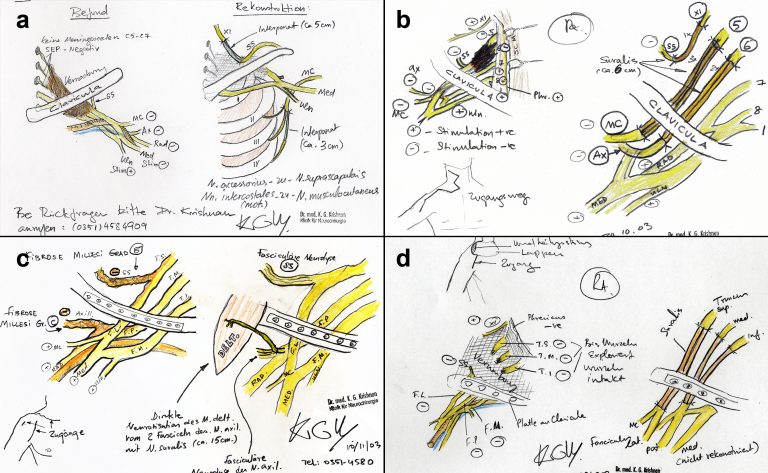
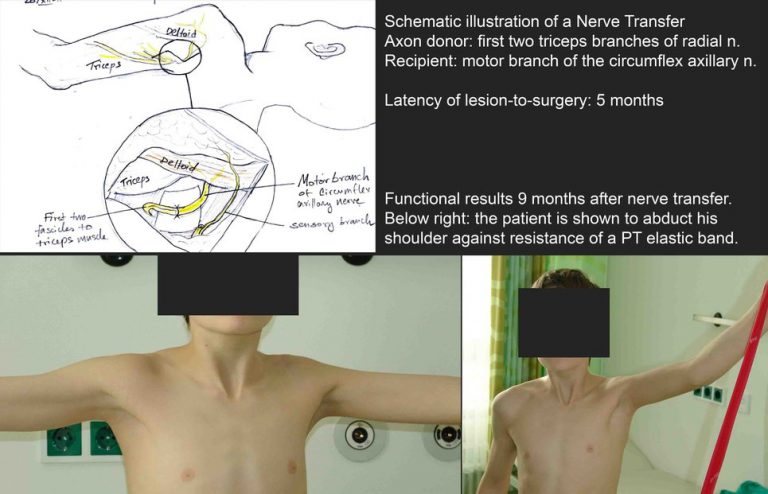
Die Rekonstruktion von Armplexusverletzungen ist von der Art und Schweregrad der Verletzung abhängig. Bei vollständigen Wurzelausrissen sollten Nervenumleitungsmaßnahmen (z.B. Rippennerven zu Armnerven) durchgeführt werden. Dadurch werden die Nervenpotentiale von einem gesunden Nerv zu dem verletzten Nerv umgeleitet. Nach solchen Operationen sind physiotherapeutische “Umlernmaßnahmen” unersetzbar.
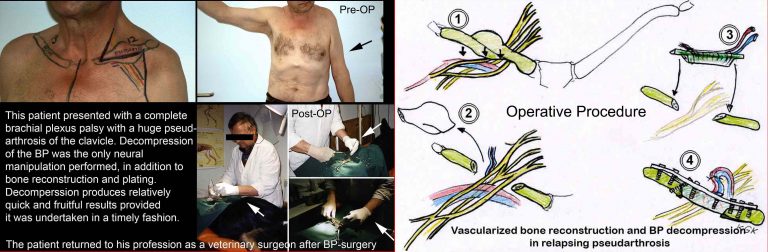
Wie bei der Rekonstruktion anderer peripherer Nerven ist das Wiedererlangen der Funktion vollständig abhängig von Art und Ausmaß der notwendigen Nervenrekonstruktion. Bei einfacher Nervendekompression (Bedrängung der Nervenfasern von Narbengewebe) ist die Prognose am günstigsten. Bei anderen Arten von Rekonstruktionen (Naht der Armplexusnerven, Nervenumleitungsmaßnahmen etc.) ist die Prognose abhängig davon, wie früh die Rekonstruktion vorgenommen wird. Das Wiedererlangen der Funktion in solchen Fällen kann unter aktiver physiotherapeutischer Maßnahmen von einem bis eineinhalb Jahre dauern.
Die Behandlung von Armplexuslähmungen erfordert eine interdisziplinäre Zusammenarbeit, wobei Spezialisten von verschiedenen Fachgebieten (z.B. Neurologen, Neurochirurgen, Physiotherapeuten, Unfallchirurgen etc.) zur Behandlung hinzugezogen werden.
- Zeitschema der Plexus brachialis Rekonstruktion:
- Offene Verletzung – Rekonstruktion möglichst sofort (abhängig vom Allgemeinstatus des Patienten)
- Geschlossene Verletzung (überwiegende Mehrheit der Fall) – Bis zu 5 Monaten unter Beobachtung bleiben à Falls keine Besserung à Primäre Nervenrekonstruktion (Nervennaht / Transplantat / NervTransfer)
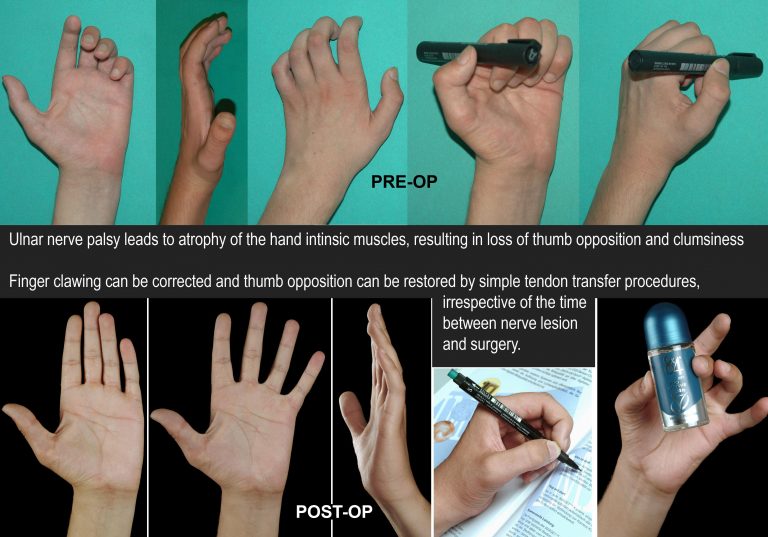
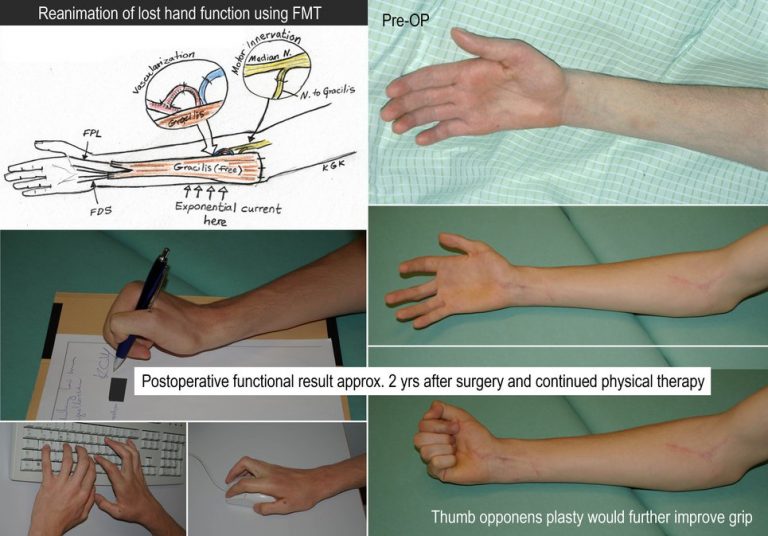
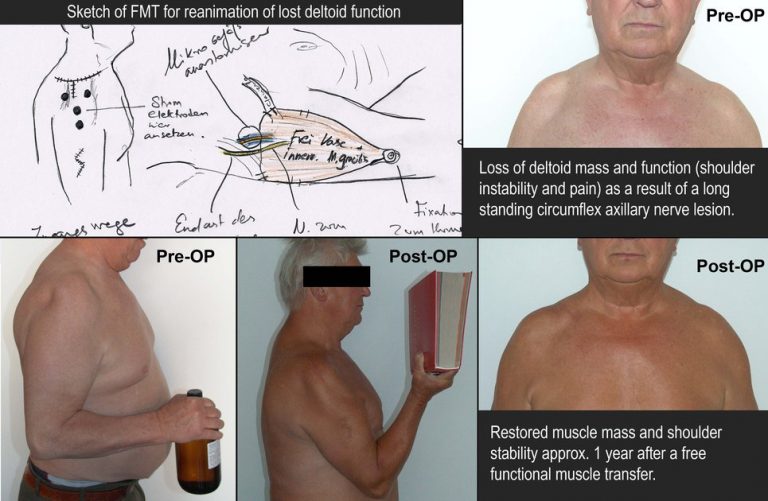
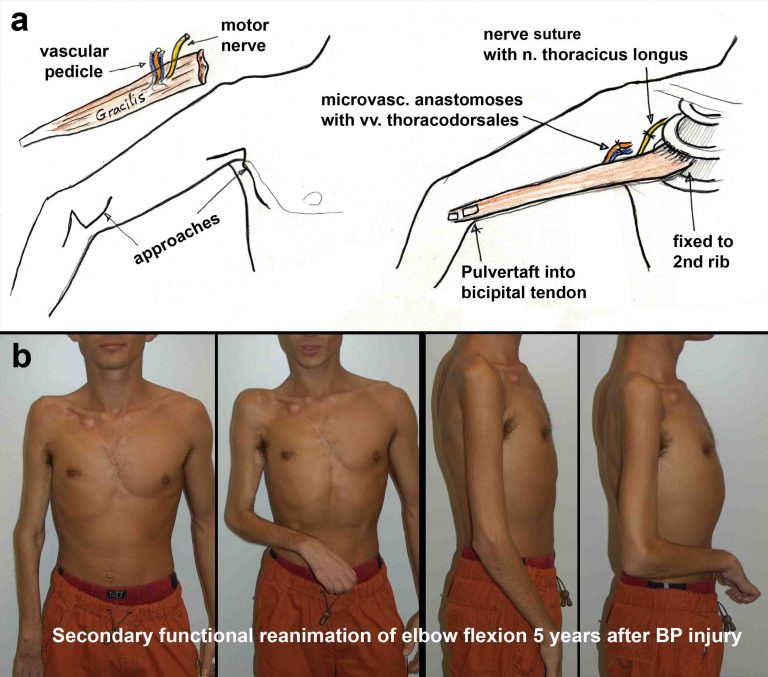
- Vorstellung des Patienten mehr als 1 Jahr – Funktionsersatzoperationen zur Widerherstellung der Beweglichkeit (Sehnentransfer, Muskeltransfer, Frei Funktionelle Muskeltransplantation FMT)
Häufig gestellte Fragen:
? Wann soll ich mich nach einer bestehenden Lähmung des Armes nach einem Unfall vorstellen?
Antwort: Möglichst sofort.
? Was sind die häufigsten Ausfälle bei Armplexuslähmungen?
Antwort: Meistens Armhebe- und -beugeparese. Abhängig vom Grad der Verletzung kann es zur vollständigen Lähmung des betroffenen Armes kommen.
? Wie entscheidet sich, ob ich mich einer chirurgischen Operation zur Armplexus- rekonstruktion unterziehen soll?
Antwort: Dies ist sehr fallabhängig. Meistens werden die Patienten, die gleich nach dem Unfall den Arzt ansprechen, bei Physiotherapeuten und Neurologen zur aktiven physiotherapeutischen Behandlung unter engmaschigen neurologischen Kontrollen vorgestellt. Die Indikationen zur chirurgischen Behandlung werden dann gestellt, wenn die Lähmung nach wie vor vollständig besteht, oder wenn es nach einer leichten Kraftverbesserung der Muskulatur zu einem Stillstand kommt. Aus diesen Gründen sollten die chirurgischen Indikationen individuell gestellt werden.
? Wie lange dauert der Krankenhausaufenthalt bei Armplexusrekonstruktionen?
Antwort: In der Regel drei bis sieben Tage.
? Wo und wie wird die postoperative Nachbehandlung durchgeführt?
Antwort: Nach der Operation werden Patienten in einer heimatnahen Rehabilitationsklinik vorgestellt, wo aktive physiotherapeutische Behandlungsmaßnahmen unter engmaschigen neurologischen und neurophysiologischen Kontrolluntersuchungen durchgeführt werden können. Es wird direkter Rücksprache mit den weiterbehandelnden Ärzten/Physiotherapeuten gehalten, sodaß eine Koordinierte Gesamtbehandlung erfolgen kann.
? Kann man bei seit längerer Zeit bestehender Lähmung des Armes noch irgendetwas tun, um die Funktion zu verbessern?
Antwort: Eine primäre Nervenrekonstruktion nach längerem Krankheitsverlauf ist wenig erfolgsversprechend, da die Zielmuskeln sich bindegewebig umgebaut haben könnten. In diesen Fällen bestehen verschiedene Möglichkeiten durch Sehnen und Muskelverlagerungen bis zur neuen autogenen Muskelaufbauplastik (der so genannte Frei Funktionelle Muskeltransfer) einige verlorenen Funktionen des Armes/Hand wiederherzustellen. Eine notwendige Bedingung hierfür ist ein passiv frei bewegliches betroffenes Gelenk.
Hier sind einige Beispiele der primären Plexus brachialis Rekonstruktion und der sekundären Funktionswiederherstellung mittels Sehnen und Muskeltransfer, bzw. Transplantation: